What is Diabetic Retinopathy?
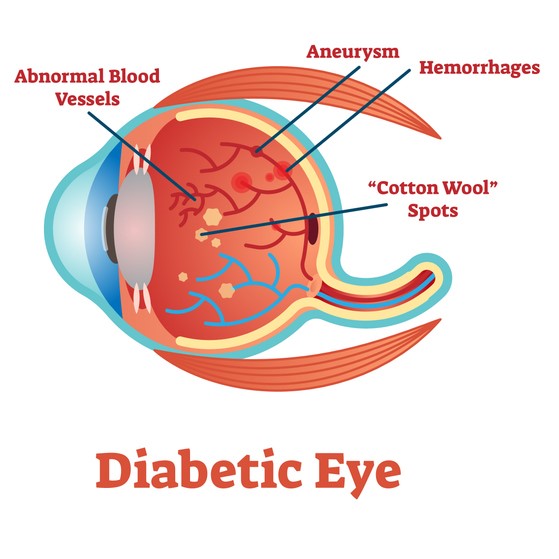
Diabetic retinopathy is caused by damage to the blood vessels in the tissue at the back of the eye (retina). Poorly controlled blood sugar is a risk factor. Early symptoms include floaters, blurriness, dark areas of vision, and difficulty perceiving colors. Blindness can occur.
Mild cases may be treated with careful diabetes management. Advanced cases may require laser treatment or surgery.
The Two Stages of Diabetic Eye Disease
There are two main stages of diabetic eye disease.
NPDR (non-proliferative diabetic retinopathy)
This is the early stage of diabetic eye disease. Many people with diabetes have it.
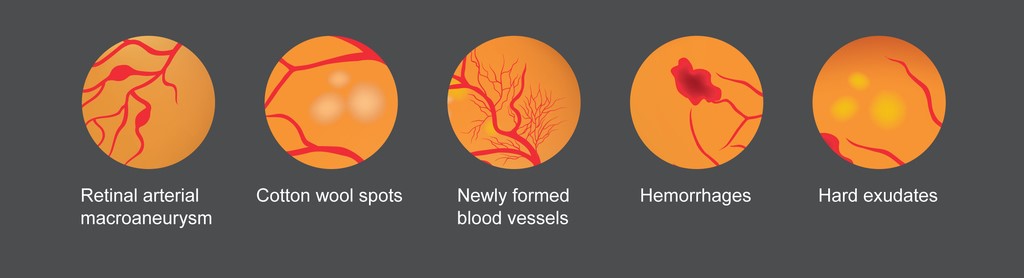
With NPDR, tiny blood vessels leak, making the retina swell. When the macula swells, it is called macular edema. This is the most common reason why people with diabetes lose their vision.
Also with NPDR, blood vessels in the retina can close off. This is called macular ischemia. When that happens, blood cannot reach the macula. Sometimes tiny particles called exudates can form in the retina. These can affect your vision too.
If you have NPDR, your vision will be blurry.
PDR (proliferative diabetic retinopathy)
PDR is the more advanced stage of diabetic eye disease. It happens when the retina starts growing new blood vessels. This is called neovascularization. These fragile new vessels often bleed into the vitreous. If they only bleed a little, you might see a few dark floaters. If they bleed a lot, it might block all vision.
These new blood vessels can form scar tissue. Scar tissue can cause problems with the macula or lead to a detached retina.
PDR is very serious, and can steal both your central and peripheral (side) vision.

Diabetic retinopathy (diabetic eye) presents itself as dark spots floating in your vision.
Diabetic Retinopathy Diagnosis
Drops will be put in your eye to dilate (widen) your pupil. This allows your optometrist to look through a special lens to see the inside of your eye.
Your doctor may do optical coherence tomography (OCT) to look closely at the retina. A machine scans the retina and provides detailed images of its thickness. This helps your doctor find and measure swelling of your macula.
Fluorescein angiography or OCT angiography helps your doctor see what is happening with the blood vessels in your retina. Fluorescein angiography uses a yellow dye called fluorescein, which is injected into a vein (usually in your arm). The dye travels through your blood vessels. A special camera takes photos of the retina as the dye travels throughout its blood vessels. This shows if any blood vessels are blocked or leaking fluid. It also shows if any abnormal blood vessels are growing. OCT angiography is a newer technique and does not need dye to look at the blood vessels.
Can Diabetic Retinopathy Go Away?
Your treatment is based on what your optometrist sees in your eyes. Treatment options may include:
Medical control
Controlling your blood sugar and blood pressure can stop vision loss. Carefully follow the diet your nutritionist has recommended. Take the medicine your diabetes doctor prescribed for you. Sometimes, good sugar control can even bring some of your vision back. Controlling your blood pressure keeps your eye’s blood vessels healthy.
Medicine
One type of medication is called anti-VEGF medication. These include Avastin, Eylea, and Lucentis. Anti-VEGF medication helps reduce swelling of the macula, slowing vision loss and perhaps improving vision. This drug is given by injections (shots) in the eye. Steroid medicine is another option to reduce macular swelling. This is also given as injections in the eye. Your doctor will recommend how many medication injections you will need over time.



















































































































